Everything You Ever Wanted to Know About DoxyPEP
Words by Daniel Hirsch
A hefty dose of antibiotics. A big syringe in the derrière. Getting treated for an STI is not fun — to say nothing of the symptoms and risks involved with contracting one like syphilis, gonorrhea, or chlamydia. With the CDC reporting rising numbers — gonorrhea is up 11% over the last five years, syphilis is up 79% — risk of infection is on the rise.
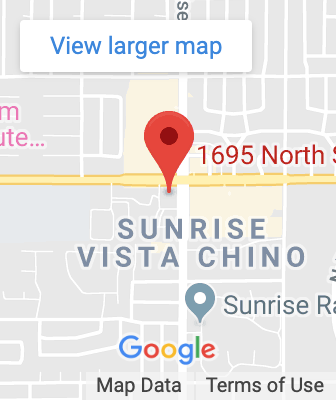
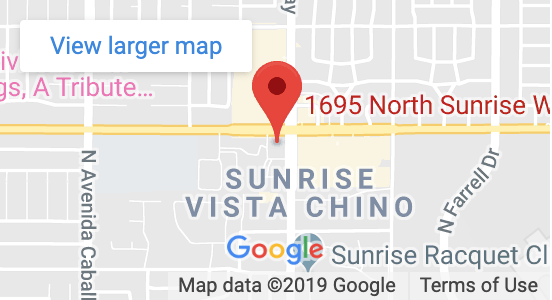
However, clinicians around the country, spurred by recently released guidance from the CDC, are recommending the antibiotic doxycycline as a means of post-exposure prophylaxis (DoxyPEP for short) to prevent the spread of STIs. I spoke with DAP Health Chief of Community Health C.J. Tobe about this prevention strategy.
Let’s start with the basics. What is DoxyPEP?
DoxyPEP, or doxycycline, is a 200 milligram pill that can be taken within 24 to 72 hours after sex. It reduces a person’s chance of contracting either chlamydia, gonorrhea, or syphilis by up to 70%. Doxycycline has been around for quite some time and is used to treat STIs and acne.
How sexually active do you need to be to justify a prescription?
It’s going to look different depending on a person’s lifestyle and the conversation with their provider. For example, if you have sex Friday, Saturday, and Sunday, you can take DoxyPEP that Monday morning and you’re good. Let’s say you’re having sex five times a week, then you should probably talk to your doctor about switching to DoxyPrEP.
And what’s DoxyPrEP?
DoxyPrEP would be taking 100 milligrams of doxycycline daily as a preventative measure. That’s typically for people who either want to make sure they’re protected, or they’re having frequent sex, or they may be a sex worker.
Are there side effects? Isn’t doxy tough on the GI tract?
A lot of the side effects that get reported are GI issues. So we recommend people take the medication with food or a carbonated drink. When people take a higher dose of doxycycline, like 200 milligrams twice a day, the side effects increase. If you go on DoxyPrEP, that’s just 100 milligrams once a day. And I can tell you it’s such a low dose that the majority of folks don’t have side effects.
One of my worst nightmares, and it’s one shared by the World Health Organization, is that an STI becomes resistant to antibiotics. Is that a concern with people regularly taking doxy?
Part of the medical community is hesitant to embrace this strategy because they don’t know what could happen in terms of drug resistance. The other half are saying, “We need to get people on it right now because it’s an important preventative tool.” There’s always going to be a risk of drug resistance when people don’t follow the dosing recommendation of a doctor. As a public health person seeing the rise in STIs, I think a patient who is having sex should have that conversation with their doctor and see if DoxyPEP is right for them. Personally, I’ve been on doxy since 2020 and it’s been a lifesaver.