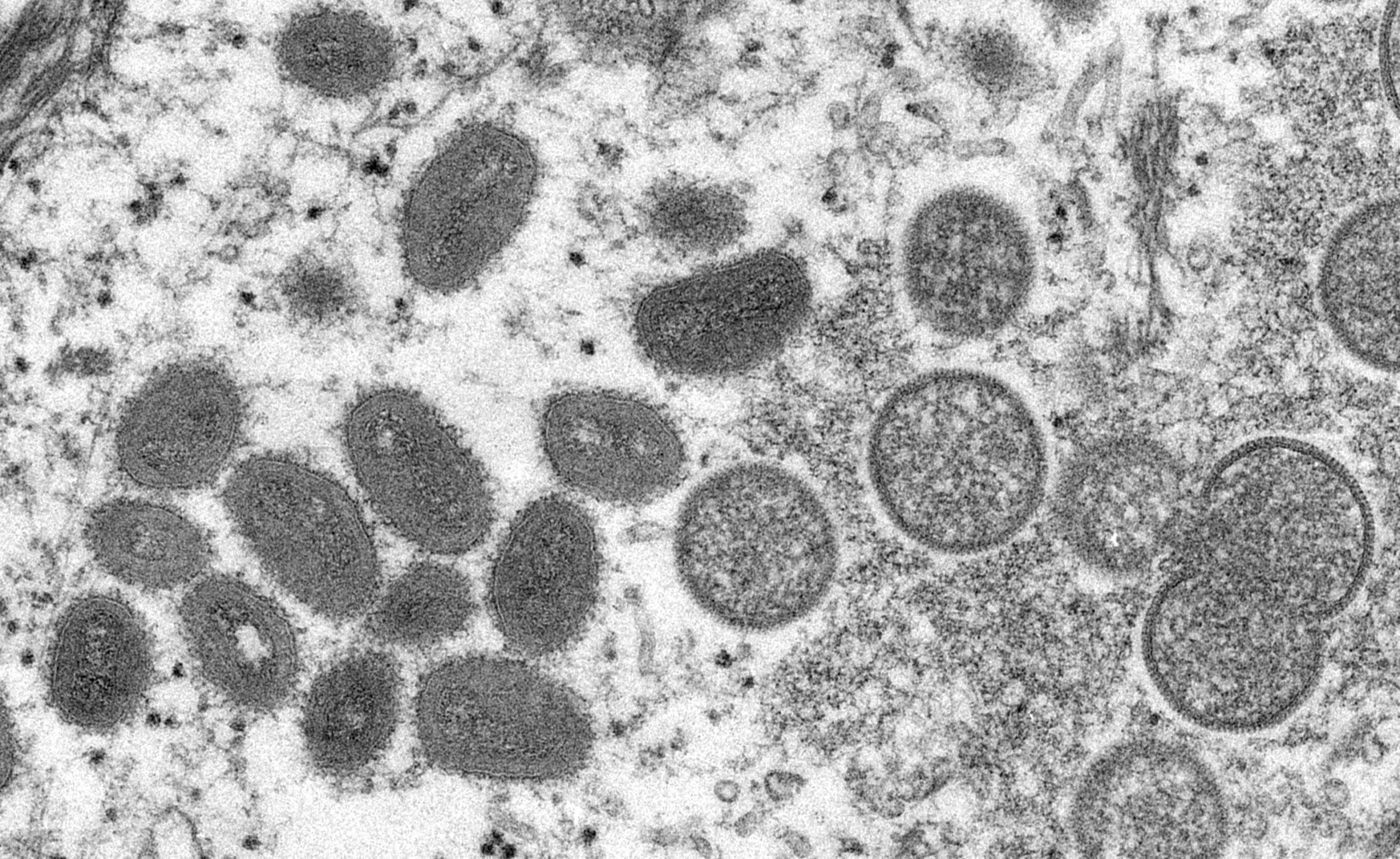
Anyone can get monkeypox. It is important we do not create stigma during this current outbreak
Transmission of monkeypox can occur with skin-to-skin contact, including sexual contact, but it is not an STI
Mpox Vaccine and Testing At DAP Health
Need to get your Mpox Vaccine? DAP Health’s Sexual Wellness Clinics continue to offer Mpox vaccines to the community at no cost, simply call to make an appointment for your vaccine today. Vaccination is highly recommended for prevention. No additional booster doses are recommended after you have received the two-dose initial series.
Having Possible Mpox Symptoms? DAP Health’s Sexual Wellness Clinics are here to help you. If you feel you may have Mpox symptoms and need to get tested, please call us today for a full STI screening including testing of Mpox lesions.
Transmission
Mpox is known to spread through prolonged close physical contact with someone who has symptoms.
- Rash, bodily fluids (such as pus or blood from skin lesions), and scabs are particularly infectious.
- Respiratory droplets, ulcers, lesions, or sores in the mouth can also be infectious, meaning the virus can spread through saliva.
- Clothing, bedding, towels, or objects like eating utensils/dishes that have been contaminated with the virus can infect others.
- People who closely interact with someone who is infectious, including health workers, household members, and sexual partners are at greater risk of infection.
- The virus can also spread from someone who is pregnant to the fetus from the placenta, or from an infected parent to child during or after birth through skin-to-skin contact.
It is unclear whether people who do not have symptoms can spread the disease.
Symptoms
Symptoms include rash, headache, fever, muscle and body aches, swollen lymph nodes, and back pain. The CDC recommends that anyone with a new or unexplained rash get checked by a medical professional.
Prevention
While the vaccine is effective in preventing illness from an exposure, it is possible to still be infected. However, symptoms generally are milder and the illness resolves in relatively shorter period than those unvaccinated.
Mpox can be transmitted through skin-to-skin contact which includes sexual contact. Prevention includes avoiding physical contact with someone who knows they have Mpox or who has a rash or skin lesions that may be associated with Mpox.
Testing
If Mpox is suspected, diagnostic samples must be collected from the suspect rash. The Clinician’s will take a swab of the fluid of vesicles, pustules, or dry crusts. Samples are sent to LabCorp for processing.
Treatment
Treatment is available through DAP Health in association with Riverside County Department of Public Health.
Trusted Sources of News and Updates:
California Department of Health