Semper Gumby
In English, the Latin unofficial motto of the U.S. Navy translates as “Always Flexible.” It perfectly describes DAP Health’s new Chief Medical Officer Dr. Joseph Aquilina
Words by Kay Kudukis
His parents were first-generation Sicilian-American, so of course the entire family went to Grandma’s house for Sunday sauce. It was a nice break from the other six days when, evenings and after school, the three kids helped Mom and Dad in the family’s cleaning business. Cleaning neither garments nor houses. Car dealerships and fitness centers — any business in Buffalo that hired them. In addition, Dad worked two more jobs hoping to give his kids a better version of the American dream than his.
Joseph Aquilina, the only boy, a middle child, took up trombone and football. Maybe because he had an interest, or maybe because after school extracurriculars were more fun than cleaning. But he was drawn to the social aspects, the camaraderie. He even ended up combining both activities when the band performed at Rich Stadium for a Buffalo Bills game. Quite a score for the teenager.
Young Joe played offensive guard and defensive end in high school football. Generally, those positions had a heavier body type than that of Aquilina, who’d grown tall but not thick. His build was more like a quarterback, or a tennis player. He picked up the racket when he was stationed in London, but more on that later.
Because of his size, Joe worked harder to stay on the team, and can still recall the fantastic feeling at homecoming when they called his name: “Playing first string, defensive end, Joseph Aquilina.”
College Bound
Some plan their post-secondary life and know exactly where they’ll be after their senior summer. Others haven’t a clue. Aquilina fell into the latter category. He thought he might like to go to college — that’s what all the kids in his honors classes were doing — but he didn’t quite know how he was going to do that. His sister had been the first of any generation to attend college, but she stayed local. He did not want to do that.
His parents didn’t have the knowledge or funds to assist, so he relied on his friends for help and ideas. The University of Rochester came up, so he applied and received academic scholarships. Bonus: It was 90 miles away from Buffalo. Far enough away to live on campus, yet close enough to bring his laundry home on the weekends. “I thought I was busting out,” Aquilina says with a laugh.
He loved Rochester. “I had such a sense of independence. You can control your own schedule. I got my first non-family job at the Fine Arts Library. It was wonderful. I was a gallery guard. I could do my homework, watch the art exhibit, make sure no one touched anything, and get paid to study.”
Life in the Lab Was Too Boring
He chose microbiology as a major, but discovered the monotony of the lab didn’t really suit him. That was a problem. One day, a solution walked in: Urologist Dr. Bob, who came to take his wife (head of the lab) to lunch. “He was an affable, gregarious, fun guy,” Aquilina recalls. “And I just asked, ‘Hey, Dr. Bob. Can I join you one day, kind of see what your day is like?’”
Dr. Bob was equally as affable at work with patients, nurses, and staff. “Everybody knew and liked him. I thought, ‘I could do this,’” Aquilina grins, remembering. “It just seemed like a very social, fun job, and he really enjoyed it. So I thought maybe I should consider medical school. I had no idea what that meant.”
His counselor knew, and the news was good. Aquilina already had most of the credits needed. He just had to take the MCAT. His score did not disappoint. He was going to be a doctor!
In the Navy
His father wanted to mortgage the family home to pay for it, which terrified Aquilina. “What if I fail? Then he’s gonna lose the house. No way.” He had friends in ROTC at Rochester. “I thought, ‘Well, they seem like they’re happy.’” He cold-called the Navy. The recruiter couldn’t believe his luck. “Yes, we’ll absolutely pay for medical school. When can you start?”
Aquilina graduated from Loyola’s Stritch School of Medicine in Chicago in May of 1994. In July of 1995, he reported for flight surgeon training at Naval Operational Medicine Institute in Pensacola.
For the two years he worked as a flight surgeon, he was deployed for six months on the USS Tarawa, attended to 500 Marine flyers, got a pilot’s license, and logged more than 300 flight hours in a CH46 helicopter.
He got married, they had twin daughters, and he continued to move up in positions and responsibilities within the Navy’s medical sector. That included three years in the U.K., and six months deployed in Kuwait before returning to San Diego. There he earned his MBA, explored his tech fascination with a “side hustle” in dental charting software while concurrently wrapping up his 22 years of service as the director of outpatient health clinics.
In Uniform No More
Now both single and a civilian, Aquilina was ready to explore different opportunities. He worked in business development for a year, then shifted back to a team environment overseeing larger medical groups and implementing new initiatives.
For eight years, he served on the board of Glenner Memory Care Centers, specializing in adult day care centers and family resources, becoming well-versed in the workings of nonprofits.
If you peep his social media, you’ll see his playful side: goofy pictures with his kids, visits to tennis matches, and adventures in sailing. In 2014, he met his now fiancé, a concierge physician in San Diego. Last summer, Dr. Joe was a tennis coach for the Special Olympics.
At Long Last, DAP Health
When he learned of DAP Health’s merger with Borrego Health, he saw a unique opportunity. “It’s a beautiful mission, and that was a huge attraction for me,” he says. “It seemed like an organization that really lived its values, which was really, really enticing.”
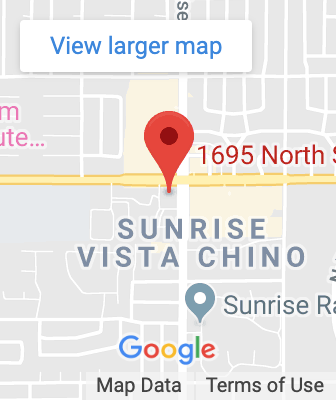
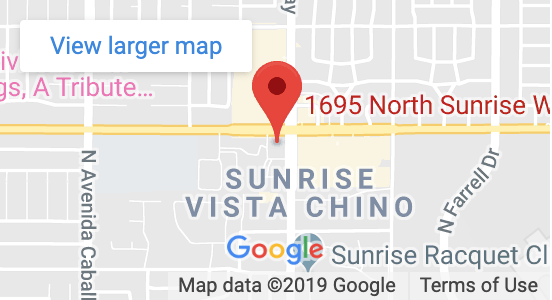
Right now, he splits his time between San Diego and Palm Springs, and his personal needs are simple: tennis partners. He says he ranks himself a solid 4.0, but “I will play whenever, wherever, with whomever.”
Semper Gumby.